The healthcare industry is constantly evolving. Scientific research spurs on new discoveries, techniques, surgeries and cures. The economic environment dictates the distribution of healthcare. In the present day and age, there are many “what-if’s” about how and to whom healthcare is delivered. This post is not intended to be an epic dissertation on healthcare in America. The purpose, rather, is to explain to those inquiring why we are no longer pursuing medical care for our pregnancy in Madison, WI.
Upon learning that we were pregnant with quintuplets, the initial meetings with our fertility specialist and perinatologists were an emotional undertaking, to say the least. These medical specialists fought long and hard to convince us to pursue multi-fetal reduction. They wanted us to take the five and reduce to 2, maybe 3. This was never an option for us, and we made it very clear from day one. However, despite our stance, the perinatologists would not discuss a plan of care with us for over a month under their supervision.
Finally, nearly two months into our pregnancy we were able to sit down and discuss how we were going to make our pregnancy a success and give our unborn children the best chance at a happy and healthy life. We came prepared to this meeting, well read on terms and proactive treatments and even brought along a few research articles to discuss. The docs may have been a bit thrown off; one was not even prepared to discuss how to combat pre-term labor. Luckily, his colleague was.
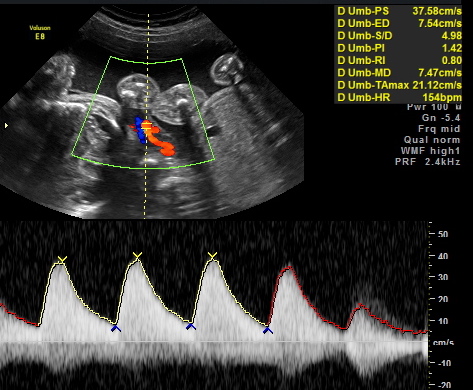
We had a long conversation about what their practice was willing to provide and what they were not. They were willing to provide monitoring prior to 24 weeks of gestation, which simply meant monthly ultrasounds. They were willing to provide a nutrition consult with their dietitian and psychological care with their social worker. But, they were not willing to consider preventative measures, and what I would consider proactive care. Despite the research I held in my hand, they would not acknowledge the efficacy of a cerclage (stitching of the cervix), non-stress testing (contraction monitoring), intensive tocolysis (treatment of contractions to delay labor), or even bed-rest. Instead they encouraged me to continue to take my prenatal vitamin and told me it was fine to exercise up to 30 minutes a day.
This information did not sit well with me, so I reached out to other mothers of quints and they were appalled. They encouraged us to get a second opinion and quickly. I didn’t at that point. I decided that I needed to come to trust my current healthcare practitioners; I did not want to seek care elsewhere knowing: 1) This would mean leaving home and 2) Our insurance would not cover it.
Then, at 18 weeks we sat across the table from another perinatologist from the same practice and a clinical nurse specialist. They informed us that we would most likely lose this pregnancy in the next 3-4 weeks. I asked and begged for them to reconsider a cerclage, and they said it would not help but would actually put me in more danger of losing my pregnancy. They shared that cerclages are only provided to persons with incompetent cervixes, which is a diagnosis typically given to moms only after having a previous miscarriage prior to 24 weeks. He told us not to give up hope but that there was essentially nothing else we could do. He encouraged me to continue to eat right and said I could still exercise up to 30 minutes daily. I asked about bed rest, tocolytic drugs and contraction monitoring and was once again told these treatment options would be of no help. Then, came the moment I realized that care at this clinic was not our only choice. I sought a second opinion.
The second opinion came from a renowned high-risk perinatologist in Arizona, who many other quint mom’s highly recommended and adored. They loved him for a very important reason; he saved their pregnancies. After a 30-minute phone call with this doc, also known as the, “Quad God,” I learned that if I didn’t have a cerclage within the next 3 days, we would, in all likelihood, lose our babies. He had a recipe for success that was incomparable to other docs’ practices due to his extensive experience with high order multiples. He has delivered 101 sets of quadruplets, 15 sets of quintuplets and 2 sets of sextuplets. To put that in perspective, our previous docs had delivered just 1 set of quads, no quints, and no sextuplets. Additionally, the average gestational age of quints delivered under his care is 33 weeks and 1 day… Academic research indicates the total population gestational average is somewhere between 25 and 27 weeks. The “Quad God’s” success was quite simply unheard of.
The next few days flew by as we attempted to plead with our insurance company to cover this care. However, to this day, they continue to deny us because:
- The services requested are/were with a non-participating provider.
- The services are/were not medically indicated because they are not appropriate to treat the condition and do not represent the standard of care to treat the condition.
- The utility of prophylactic cerclage is unproven and there is evidence to suggest it may be detrimental and may be associated with an increase in preterm delivery and pregnancy loss.
However, here I sit to write this post at 24 weeks- 6 weeks later- with healthy babies developing within me.
So, many ask why am I still here? I have the cerclage, the pregnancy is stable and insurance continues to not be willing to pay a dime towards our care. Why would I not come back to Madison?
The answer to me is plain and simple:
1. There were no other participating providers in our insurance network besides our initial maternal and fetal medicine specialists.
We were concerned with the care that was being provided by our previous providers for several reasons, including their unwillingness to consider preventative and proactive measures of care. Even after the cerclage, they informed me that they would be unwilling to provide intense tocolysis, contraction monitoring and support strict bed rest. I have been receiving these treatments here in AZ since the moment I arrived.
2. Emergent care, via cerclage, strict bed rest, contraction monitoring and tocolysis, were/are all required and medically indicated, in order to, prevent pre-term labor.
There is a body of research, which supports these facets of care during multi-fetal gestation. Additionally, a cerclage is not an “experimental therapy” but again is considered a component of normal perinatal care in a high-order multiples pregnancy.
My current perinatologist has published over 25 peer-reviewed articles on the management of high-order multiples and has delivered 15 sets of quintuplets whom have exceeded the average gestational age by over 5 weeks. The previous specialists have never delivered, or managed, a quintuplet pregnancy and while they are revered clinicians in their areas of research, they have not published on the management of high-order multiple pregnancies.
The peace that I feel in pursuing treatment under this new doctor’s care is overwhelming. For the first time in this pregnancy, I am confident in the care that I am receiving. I would fear for the well being of my babies if they were subject to the care of the practitioners in Madison. They have not demonstrated that they truly care about our five miracles, nor do they appear willing to proactively fight for a healthy pregnancy.
Unfortunately, these reasons are not convincing to our insurance provider. Therefore, we will continue to appeal and grieve this process with them, as we have since we initiated care outside of network. It is truly unfortunate that we cannot find comparable care within our insurance providers network. Our current doctor even offered to communicate his care plan to our previous docs, so that we could remain in-network, however they have denied all collaboration at this point.
Our biggest concern at this point, outside the healthy delivery of our 5 babies, is the financial livelihood of our family. The medical practitioners we are working with are very cognoscente of our financial situation and have been more than accommodating. But, we know that once I am admitted for closer monitoring and more intense treatment, the bills will begin to accumulate. Then, of course, will come the likely astronomical Neonatal Intensive Care Unit bill for 5 babies.
And so, we are witness to the cost of good healthcare in America. Still, we are simply unwilling to sacrifice our right to choose a qualified practitioner just because an insurance company is holding us financially hostage. We feel as parents-to-be that we now represent our children; we are now responsible for their well being until they are able to take on that responsibility themselves. We will fight, and continue to fight, for our children’s God given right to life, liberty, and the pursuit of happiness.